As a surgeon, I often meet patients who ask, “Doctor, why is my wound taking so long to heal?”
The answer almost always comes down to one vital factor — oxygen delivery and healing are inseparable. Every cell in your body depends on oxygen to survive, but during recovery, its need multiplies. Oxygen fuels the energy your tissues require to rebuild collagen, fight bacteria, and form new blood vessels. Without enough oxygen reaching those fragile areas, healing slows, and wounds may stay open or painful for weeks.
In my clinical experience at Care Well Medical Centre, Delhi, I see how patients with diabetes, smoking habits, or poor circulation often struggle because their tissues simply do not receive the oxygen they need. When we correct that oxygen delivery — naturally or through medical therapy — their recovery improves dramatically.
If you wish to understand the therapy that enhances this process in a controlled way, you may read our detailed guide — What Is Hyperbaric Oxygen Therapy?.
The Science of Oxygen and Tissue Repair
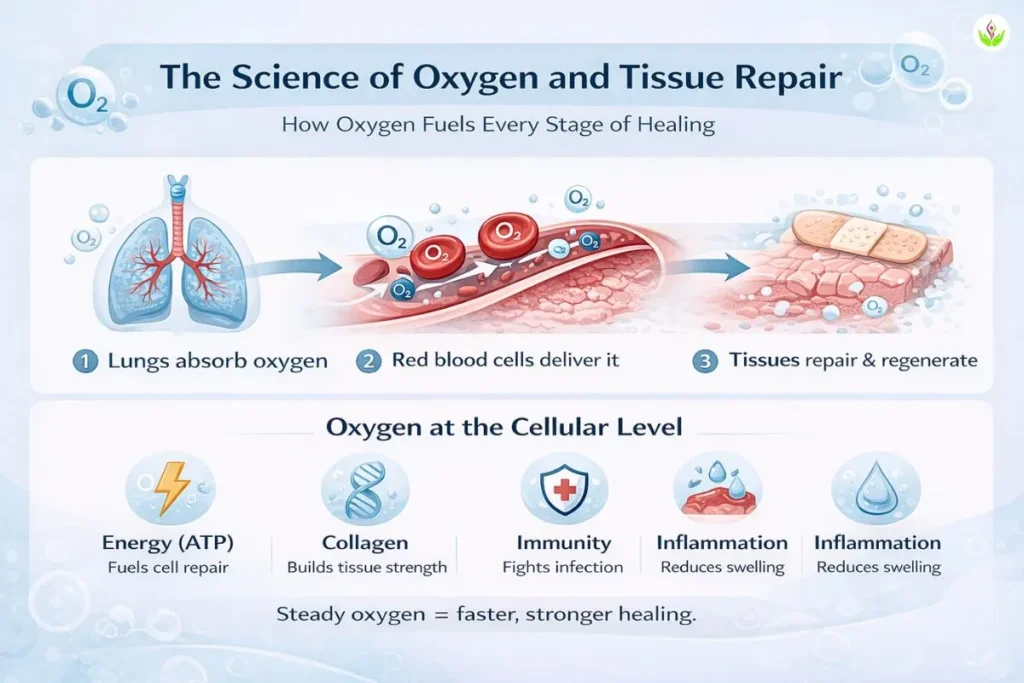
The importance of oxygen in tissue repair cannot be overstated. Every phase of healing — from inflammation to new tissue formation — depends on how well oxygen reaches and nourishes the affected cells. When oxygen delivery is optimal, wounds close faster, scars mature better, and infection risk decreases. When it is poor, the healing process stalls, even if other treatments are ideal.
How Oxygen Reaches Your Tissues
When you breathe, oxygen passes into your lungs and binds with haemoglobin in red blood cells. These cells transport oxygen to tissues that need repair, while a small portion dissolves directly into your plasma — this helps reach deeper or poorly perfused wounds.
In simple terms:
- Red blood cells: Carry most of the oxygen bound to haemoglobin.
- Plasma oxygen: Dissolves directly in blood fluid and diffuses into hard-to-reach areas.
- Why it matters: Injured tissue often has poor circulation, so boosting plasma oxygen (as in HBOT) ensures oxygen still arrives where it is needed most.
Cellular Use of Oxygen During Healing
Once oxygen reaches the wound, cells use it for key repair processes:
| Healing Function | Oxygen’s Role |
| Energy production (ATP) | Fuels cell division and tissue regeneration. |
| Collagen synthesis | Builds stronger, flexible scar tissue. |
| Immune response | Helps white blood cells kill bacteria and control infection. |
| Inflammation control | Reduces swelling and promotes clean wound edges. |
In my clinical experience at Care Well Medical Centre, wounds that receive steady oxygen supply show faster closure and less scarring.
When Oxygen Delivery Drops — Healing Slows
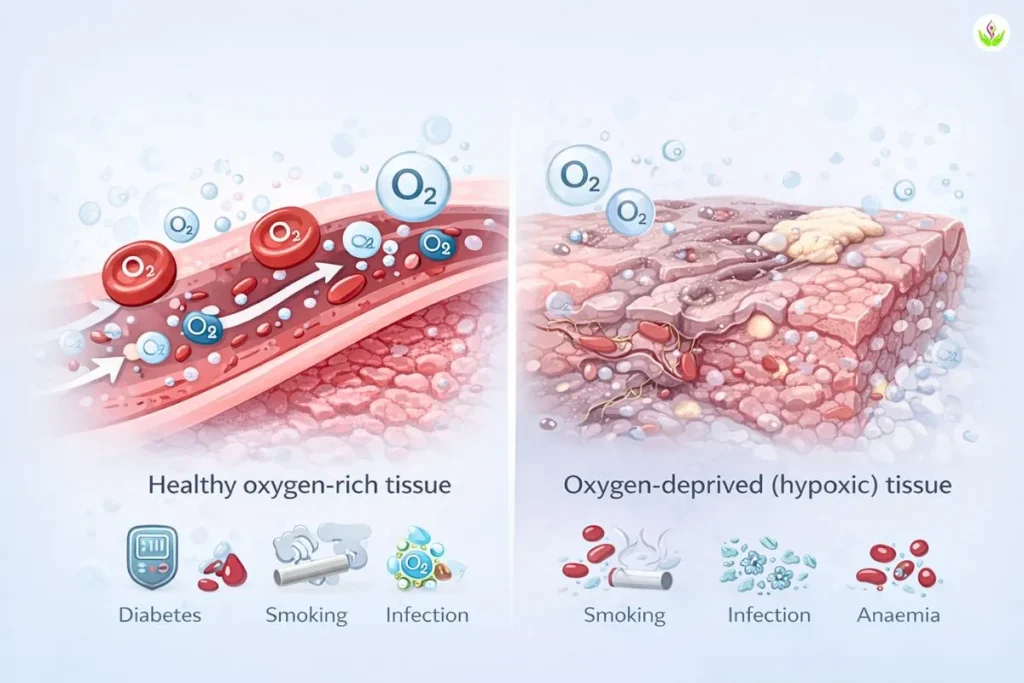
In every stage of recovery, oxygen acts as the silent driver of progress. When its supply falls below what tissues require, a condition called hypoxia, the result is delayed healing. Cells struggle to produce energy, collagen weakens, and the body’s ability to fight infection diminishes. Even well-planned wound care cannot succeed if oxygen delivery remains poor.
Common Causes of Poor Oxygen Delivery
Several everyday health conditions can quietly limit how much oxygen reaches your wound:
- Diabetes: High blood sugar damages small blood vessels, reducing blood flow and slowing tissue repair.
- Smoking: Nicotine narrows blood vessels and carbon monoxide blocks oxygen from binding to haemoglobin.
- Infection: Swelling and pus compress blood flow, trapping oxygen away from healing tissue.
- Anaemia: Low red blood cell count means there are fewer carriers to deliver oxygen to your cells.
Even environmental factors such as pollution or poor circulation from sitting too long can further reduce oxygen availability.
In my clinical experience at Care Well Medical Centre, Delhi, many chronic wounds fail to progress until we correct these underlying factors through improved oxygen delivery and blood flow support.
What Your Wound Looks Like When Oxygen Is Low
You can often recognise oxygen deficiency by the way a wound behaves or appears:
| Sign | Typical Observation |
| Pale or dusky wound edges | Tissue lacks healthy pink colour due to poor blood flow. |
| Slow or absent granulation tissue | The red, bumpy healing tissue does not form properly. |
| Increased or foul-smelling discharge | Indicates bacterial overgrowth and poor oxygenation. |
| Delayed scab formation | The wound remains open or moist for longer than expected. |
When I see these signs in patients, my first thought is to assess circulation and oxygen status before increasing any topical or antibiotic treatment. Once oxygen levels improve, these wounds often begin to respond within days.
How Better Oxygen Delivery Speeds Up Healing
When oxygen reaches the wound in sufficient amounts, healing moves from struggle to progress. Every extra molecule of oxygen fuels cellular energy, helps new blood vessels grow, and supports the natural defences that prevent infection. Simply put, the better your oxygen delivery, the stronger your body’s ability to repair itself.
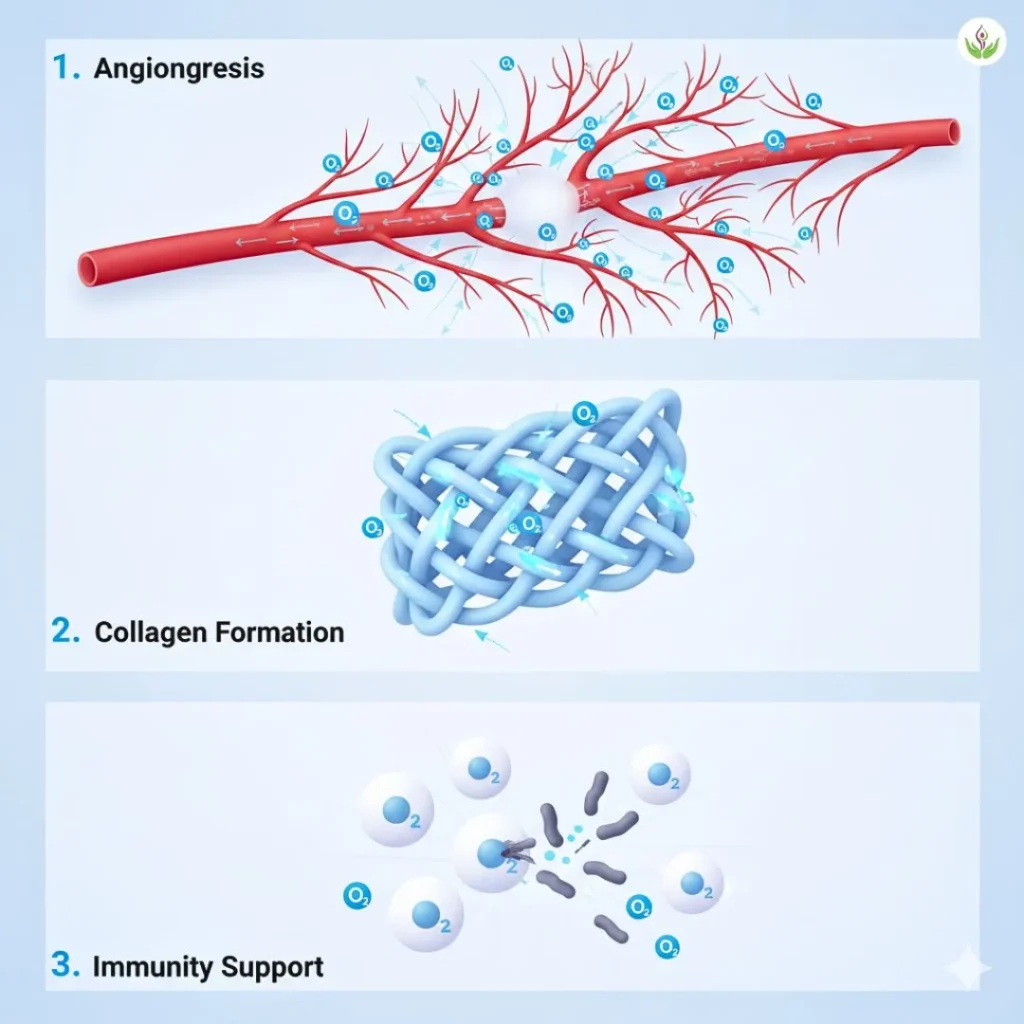
Oxygen and Angiogenesis (New Blood Vessel Formation)
Oxygen stimulates the release of growth factors that signal new capillaries to form around injured tissue. This process, called angiogenesis, improves circulation and ensures a continuous supply of nutrients and immune cells to the wound site.
- High oxygen = more microvessels that sustain tissue regeneration.
- Low oxygen = stagnant healing, as old or damaged vessels fail to expand.
In advanced wound therapies like Hyperbaric Oxygen Therapy (HBOT), pressurised oxygen enhances this process, allowing oxygen to diffuse deeper into tissues that normal blood flow cannot reach.
Oxygen and Collagen Formation
Collagen acts as the structural “scaffold” for new skin. Its production depends heavily on oxygen. Without enough oxygen, collagen fibres form weakly and the wound may reopen or scar irregularly.
Key roles of oxygen in collagen repair:
- Activates enzymes (prolyl and lysyl hydroxylase) that build strong collagen cross-links.
- Supports fibroblast cells — the main builders of connective tissue.
- Reduces fragile scar tissue and improves wound tensile strength.
Oxygen and Immunity in Wound Recovery
Your immune cells rely on oxygen to kill harmful bacteria and clear debris.
- Neutrophils use oxygen to create reactive molecules that destroy infection-causing microbes.
- Macrophages require oxygen to digest dead tissue and signal new tissue growth.
When oxygen is scarce, bacteria multiply faster than the immune system can respond, delaying closure and increasing pain or discharge.
In my clinical experience at Care Well Medical Centre, Delhi, patients who receive timely oxygen-boosting interventions—whether through improved circulation, breathing therapy, or HBOT—often notice visible healing progress within the first few sessions.
Clinical Methods to Improve Oxygen Delivery
Your recovery depends not only on medical treatment but also on how well your body can deliver oxygen to its tissues. Whether you are healing from surgery, trauma, or a chronic wound, improved oxygen delivery for recovery helps cells repair faster and resist infection. In practice, this means optimising both your body’s natural oxygen supply and, when necessary, using advanced medical methods to boost it further.
Lifestyle and Medical Optimisation
Even simple, everyday choices can significantly enhance oxygen circulation and tissue repair. In my clinical experience, patients who combine medical therapy with these practices heal more predictably:
- Hydration: Water thins the blood slightly, allowing oxygen to travel more efficiently through small vessels.
- Nutrition: Iron, vitamin C, and protein support haemoglobin production and collagen repair.
- Circulation: Gentle walking, leg elevation, or physiotherapy improve blood flow in oxygen-starved tissues.
- Breathing practices: Deep diaphragmatic breathing or guided exercises increase lung capacity and oxygen exchange.
These habits create a stable internal environment where medical therapies can perform at their best.
Medical Interventions
When lifestyle measures are not enough, targeted oxygen-based treatments can directly raise tissue oxygen levels:
| Therapy Type | How It Works | Typical Use |
| Topical oxygen therapy | Delivers oxygen directly onto the wound surface through a sealed dressing. | Suitable for small ulcers or diabetic wounds. |
| Systemic oxygen therapy | Uses nasal cannula or mask to increase oxygen concentration in the bloodstream. | For general oxygen support or mild hypoxia. |
| Hyperbaric Oxygen Therapy (HBOT) | Exposes the patient to 100 % oxygen at higher pressure, saturating both red cells and plasma. | For chronic, non-healing, or radiation-injured tissues. |
Each option has specific indications, and a doctor determines which is safest after assessing your lung function, circulation, and medical history.
To understand how HBOT differs from normal oxygen therapy, read Oxygen Under Pressure vs Normal Oxygen Therapy — it explains why pressurised oxygen often achieves results that standard methods cannot.
Why HBOT Provides Superior Oxygen Delivery
Many patients ask me how hyperbaric oxygen therapy (HBOT) differs from regular oxygen treatment. The key difference lies in pressure. In normal oxygen therapy, you breathe oxygen through a mask at room pressure. In HBOT, you sit in a sealed chamber where oxygen is given at 2–3 times the normal pressure, allowing your lungs to absorb far more oxygen. This extra oxygen dissolves in your blood plasma and reaches tissues that red blood cells cannot — making HBOT more effective for slow-healing wounds.
Pressurised Oxygen Mechanics
Under high pressure, oxygen does not depend only on red blood cells for transport. It dissolves directly into plasma and diffuses deep into oxygen-starved tissues.
| Mechanism | Normal Oxygen Therapy | HBOT |
| Pressure level | 1 atmosphere | 2–3 atmospheres |
| Oxygen concentration | Up to 100 % | 100 % under pressure |
| Oxygen in plasma | Minimal | Greatly increased |
| Tissue reach | Only areas with good circulation | Deeper, poorly perfused tissues |
This deeper oxygen reach supports cell repair, new blood vessel formation, and infection control — all essential for recovery.
Typical HBOT Outcomes and Clinical Evidence
According to the Undersea and Hyperbaric Medical Society (UHMS), HBOT has shown clear benefits in:
- Faster wound closure in diabetic and radiation-injured tissues.
- Reduced inflammation and swelling.
- Improved collagen formation and stronger healing edges.
At Care Well Medical Centre, Delhi, patients often notice visible wound improvement within 5–10 HBOT sessions — healthier colour, less discharge, and reduced pain.
To learn how the process works step by step, see our explainer — HBOT Explained in Simple Medical Terms.
Oxygen Therapy Cost in Delhi and Accessibility at Care Well Medical Centre
Patients often ask about the practical aspect of treatment — especially the oxygen therapy cost in Delhi and how easily it can be accessed. The cost of Hyperbaric Oxygen Therapy (HBOT) varies depending on the facility, the type of chamber used, and the number of sessions needed for complete recovery.
Typical Cost and Treatment Course
| Treatment Factor | Range / Detail (Approx.) |
| Cost per session (Delhi NCR) | ₹6,000 – ₹12,000 per session |
| Recommended sessions | 20 – 40 sittings for chronic or slow-healing wounds |
| Session duration | 60 – 90 minutes inside the chamber |
| Estimated total cost | ₹1,20,000 – ₹4,80,000 (depends on condition and progress) |
Most patients begin noticing visible wound improvement and reduced discharge within 8–12 sessions, although a full treatment course is generally required for lasting recovery.
At Care Well Medical Centre, Delhi, HBOT plans are individualised after medical evaluation, ensuring each patient receives the right number of sessions for their condition.
Accessibility at Care Well Medical Centre
Located in South Delhi, Care Well Medical Centre offers fully monitored, medically certified HBOT chambers in a controlled and comfortable environment. The centre is easily accessible from Delhi, Gurugram, and Noida.
Before therapy begins, every patient undergoes a pre-treatment evaluation that includes:
- Checking blood sugar, haemoglobin, and blood pressure
- Assessing ear pressure tolerance
- Reviewing lung health and medications
These steps ensure HBOT is safe, effective, and tailored to your overall health.
Delhi’s high pollution levels and humid climate can sometimes slow wound healing. By increasing oxygen concentration and circulation, HBOT helps overcome these challenges and supports steady recovery in urban environments.
Doctor’s Note: Safety and Individualisation
Every treatment must begin with one guiding principle — safety first. While Hyperbaric Oxygen Therapy (HBOT) is widely recognised as a safe and evidence-based adjunct therapy, it is not suitable for every patient in the same way. The key lies in proper screening, personalised dosage, and careful monitoring throughout the course of treatment.
Before starting HBOT, I always perform a detailed evaluation to ensure your body can tolerate the pressure and oxygen levels safely. This includes reviewing your medical history, checking lung health, and ruling out any conditions that might pose a risk.
When HBOT Should Be Avoided (Contraindications)
Certain medical conditions require extra caution or may temporarily prevent HBOT use:
- Untreated pneumothorax (collapsed lung) — the increased chamber pressure can worsen trapped air inside the chest.
- Uncontrolled seizures or epilepsy — oxygen fluctuations may trigger seizure activity.
- Severe respiratory infections or sinus congestion — pressure changes can cause discomfort or pain.
- Uncontrolled fever or claustrophobia — may affect patient comfort and chamber tolerance.
If any of these conditions are present, treatment is postponed or modified until it is safe to proceed.
Personalised Dosage and Monitoring
At Care Well Medical Centre, Delhi, each patient’s oxygen dosage, session duration, and chamber pressure are individually set. I adjust the plan based on your age, diagnosis, wound condition, and oxygen tolerance.
During therapy, your oxygen levels, ear pressure, and comfort are continuously monitored.
This personalised approach ensures maximum therapeutic benefit with minimal side effects. Common temporary sensations — such as mild ear pressure or fatigue — usually resolve shortly after the session.
Doctor’s Reassurance
Healing with HBOT is gradual but measurable. Some patients see visible tissue improvement within a few sessions, while others need a longer course depending on circulation and overall health.
My advice is simple: be patient with your body. Oxygen does not just close wounds — it rebuilds tissue strength, reduces inflammation, and restores vitality from within. With proper screening and steady follow-up, HBOT can become a safe and valuable part of your recovery journey.
Summary: The Link Between Oxygen and Healing
Healing depends on oxygen at every step. When tissues receive enough oxygen, energy rises, inflammation settles, and recovery becomes faster. Because HBOT raises oxygen delivery, healing accelerates — especially in chronic or slow-healing wounds.
At Care Well Medical Centre, Delhi, I have seen that steady oxygen improvement leads to measurable results: stronger tissue, less pain, and visible wound closure.
To understand the therapy in detail, you may read:
- What Is Hyperbaric Oxygen Therapy?
- How Hyperbaric Oxygen Therapy Works
- Oxygen Under Pressure vs Normal Oxygen Therapy
- HBOT Explained in Simple Medical Terms
Healing is gradual, but every session brings your body closer to strength and recovery. If you are considering HBOT for chronic wounds or recovery, you can learn more about the treatment process, benefits, and safety at our main page — Hyperbaric Oxygen Therapy in Delhi.
FAQs About Oxygen Delivery and Healing
Oxygen delivery refers to how efficiently oxygen from your lungs travels through blood and reaches tissues. It fuels energy production, collagen repair, and immune activity — all essential for wound healing.
Oxygen provides the energy your cells need to grow new tissue and fight infection. When oxygen levels are high, wounds close faster and scars form more smoothly.
When oxygen delivery is poor, a condition called hypoxia develops. This slows tissue repair, increases infection risk, and causes wounds to remain red, painful, or open for longer.
Hyperbaric Oxygen Therapy (HBOT) is generally safe under medical supervision. However, patients with untreated pneumothorax, uncontrolled seizures, or severe respiratory infections must be evaluated before treatment. Proper screening ensures safety for each individual.
At clinics such as Care Well Medical Centre, Delhi, HBOT sessions typically cost ₹6,000 – ₹12,000 each, depending on the chamber type and condition treated. A full course may include 20 – 40 sessions for chronic or non-healing wounds.
Most patients need 20–40 sessions, depending on the wound type, age, and circulation. Some notice visible tissue change within 8–10 sittings, while chronic wounds require longer treatment for full recovery.
Yes. HBOT often works alongside dressings, antibiotics, or surgical care. It enhances oxygen levels in tissues, allowing other treatments to work more effectively and safely.
Mild ear pressure, slight fatigue, or temporary light-headedness may occur after a session. These effects usually resolve quickly. Serious side effects are rare when treatment is medically supervised.
Disclaimer: For educational purposes only. Individual results may vary.