When patients ask me about Normal oxygen therapy vs HBOT, the frustration is very real. They are already on oxygen, reports look acceptable, yet healing feels slow. This happens because people often misunderstand oxygen therapy as a complete healing solution, when in reality it plays only one part in the recovery process.
Normal oxygen therapy improves oxygen levels in the blood, but healing does not occur in the bloodstream. Healing happens at the tissue and cellular level, especially in areas affected by swelling, poor circulation, or long-standing damage. When oxygen fails to reach these deeper zones effectively, the body cannot recover properly, regardless of how much oxygen a patient inhales.
This is where the concept of oxygen under pressure becomes clinically important. Patients looking for clinical application and treatment details can explore our Hyperbaric Oxygen Therapy in Delhi page for a complete medical overview. Hyperbaric Oxygen Therapy uses pressure to change how oxygen behaves inside the body, allowing it to move beyond the blood and into tissues where healing actually takes place. To understand the medical foundation of this treatment in detail, you can read What Is Hyperbaric Oxygen Therapy?
Why HBOT Works When Regular Oxygen Often Fails
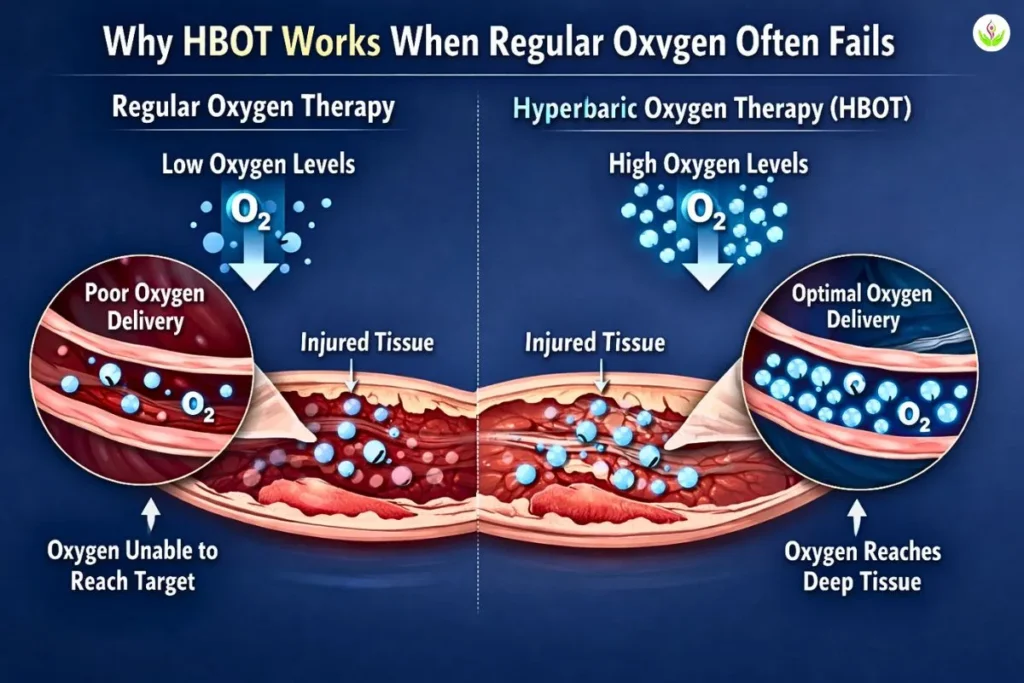
In my clinical experience, regular oxygen therapy rarely fails due to lack of oxygen. It fails because oxygen delivery is restricted. Inflammation, damaged blood vessels, and impaired microcirculation prevent oxygen from reaching the tissues that need it most, even when blood oxygen levels appear normal.
HBOT overcomes this limitation by combining oxygen with increased pressure. Under pressure, oxygen dissolves directly into plasma, making it less dependent on red blood cells and more capable of reaching low-circulation and injured areas. The practical difference is clear:
- Normal oxygen supports blood oxygen levels
- HBOT improves tissue and cellular oxygenation
- Pressure determines how far oxygen can actually travel
That single factor changes outcomes. When oxygen consistently reaches the cellular level, the body gets a genuine opportunity to repair and recover. This is why HBOT often succeeds in situations where regular oxygen therapy reaches its natural limit.
What Does “Oxygen Under Pressure” Mean?
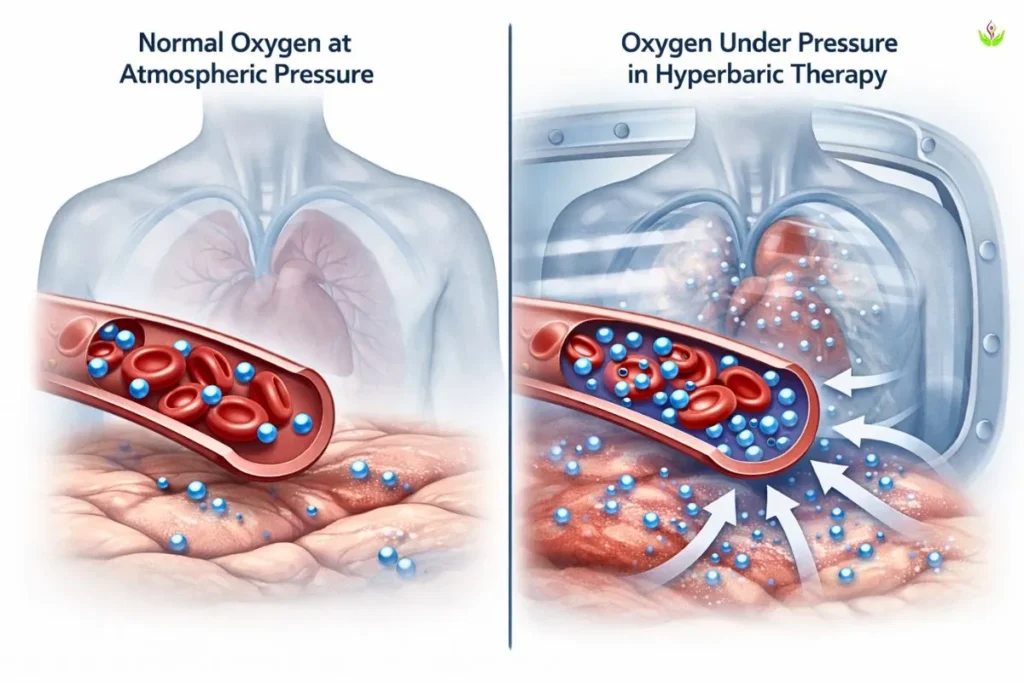
When I say oxygen under pressure, I am not talking about more oxygen alone. I am talking about oxygen delivered in a different physical environment. Under normal conditions, we breathe oxygen at atmospheric pressure, which is the pressure of air around us at sea level. This limits how much oxygen the body can absorb and how far that oxygen can travel beyond the bloodstream.
In pressurized oxygen therapy, medical teams deliver oxygen at higher-than-atmospheric pressure inside a controlled chamber. This change in pressure alters oxygen behavior inside the body. Instead of depending mainly on red blood cells, oxygen begins to dissolve directly into plasma. That single shift allows oxygen to move more freely and reach areas with swelling, poor circulation, or tissue damage.
Inside a hyperbaric chamber, pressure becomes the key driver of oxygen delivery. Higher pressure increases oxygen absorption and improves diffusion into tissues. In simple terms, pressure pushes oxygen deeper. It allows oxygen to cross barriers that normally block its movement, especially in injured or inflamed areas.
This is why Hyperbaric Oxygen Therapy is fundamentally different from routine oxygen use. The benefit does not come from breathing oxygen alone. It comes from how pressure transforms oxygen into a more powerful healing tool, without changing the oxygen itself.
HBOT vs Normal Oxygen Therapy – Core Difference
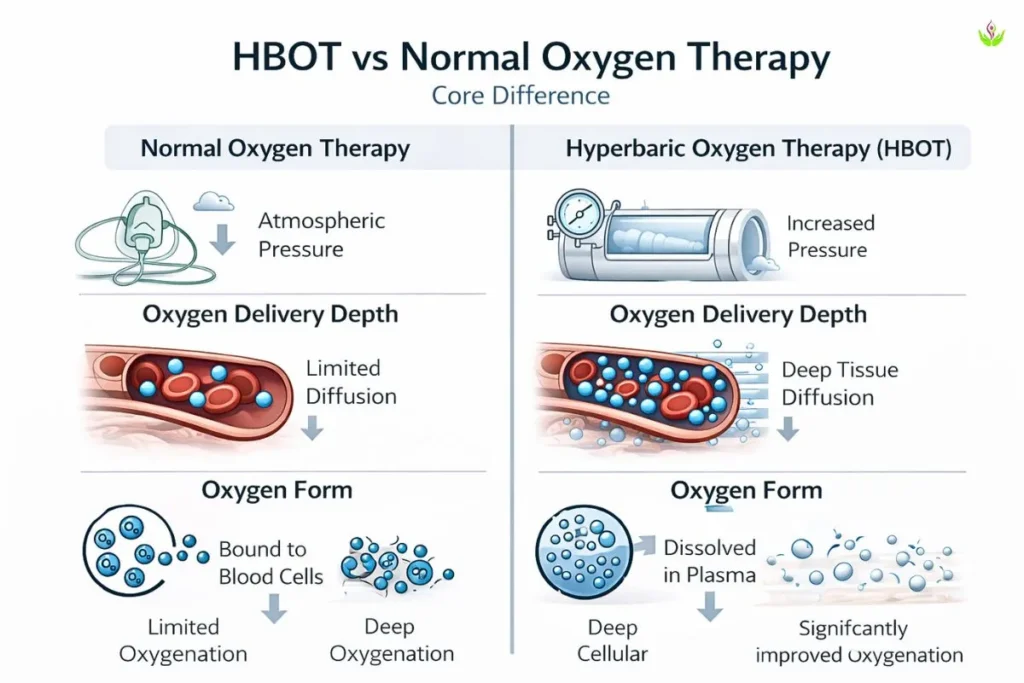
When I explain the difference between HBOT and normal oxygen therapy, I keep it practical. Both involve oxygen, but they work in very different ways inside the body. The real distinction comes down to pressure, delivery depth, and the form in which oxygen travels.
Pressure Level
Normal oxygen therapy delivers oxygen at atmospheric pressure, the same pressure we breathe every day. This limits oxygen absorption and restricts how far oxygen can move beyond the bloodstream.
HBOT uses increased pressure inside a medical chamber. That added pressure is the turning point. It changes how oxygen behaves in the body and prepares it for deeper delivery.
Oxygen Delivery Depth
With normal oxygen therapy, oxygen mainly supports blood oxygen levels. Swollen tissues and poor blood flow largely confine oxygen delivery to the circulation.
In HBOT, pressure enables oxygen delivery at the cellular level. Oxygen diffuses beyond blood vessels and reaches deeper tissues, leading to improved tissue oxygenation even in areas with compromised circulation. This depth is what supports real healing.
Oxygen Form
Normal oxygen therapy depends on hemoglobin-bound oxygen. Oxygen attaches to red blood cells, and damaged circulation limits its delivery.
Under hyperbaric conditions, oxygen becomes plasma-dissolved oxygen. This allows oxygen to travel independently of red blood cells and reach tissues that would otherwise remain deprived.
HBOT vs Normal Oxygen Therapy – Key Differences
| Aspect | Normal Oxygen Therapy | Hyperbaric Oxygen Therapy (HBOT) |
| Pressure Level | Atmospheric pressure | Increased chamber pressure |
| Oxygen Delivery Depth | Mainly limited to blood | Reaches tissues and cells |
| Tissue Oxygenation | Often restricted | Significantly improved |
| Oxygen Form | Hemoglobin-bound | Plasma-dissolved |
| Clinical Impact | Supportive | Therapeutic |
This combination of pressure, depth, and oxygen form explains why HBOT can succeed where normal oxygen therapy reaches its natural limit.
Why Normal Oxygen Therapy Often Falls Short
Clinically, normal oxygen therapy often struggles not because oxygen is unavailable, but because delivery breaks down at the tissue level. These are the most common oxygen therapy limitations I see in practice.
Why Oxygen Fails to Reach Tissues
- Swelling (Inflammation): Swollen tissues compress small blood vessels. Oxygen may circulate in the blood, but diffusion into inflamed areas remains poor, resulting in ongoing tissue hypoxia.
- Blocked Microcirculation: Reduced or disrupted capillary flow prevents oxygen from reaching cells efficiently. In such cases, oxygen therapy supports blood levels but does not work as an effective tissue hypoxia treatment.
- Damaged Capillaries: Oxygen transfer depends on intact capillary walls. When these are damaged, oxygen remains confined to the bloodstream and fails to enter surrounding tissues.
Clinical Insight
This is the key point I emphasize to patients.
Healing depends less on how much oxygen is inhaled and more on how effectively oxygen is delivered to tissues. That principle explains why oxygen delivery itself becomes the deciding factor in recovery, explored further in Why Oxygen Delivery Matters for Healing.
How Pressure Changes Oxygen Absorption in HBOT
In my clinical practice, I explain HBOT in very simple terms. Pressure changes how oxygen behaves inside the body. At normal atmospheric pressure, oxygen mainly stays bound to red blood cells. When pressure increases inside a hyperbaric chamber, oxygen dissolves into plasma and can move beyond the bloodstream. This is why pressure increases oxygen absorption and improves oxygen diffusion in tissues.
From a medical perspective, this pressure-driven delivery becomes crucial in injured or poorly supplied areas. Swelling and vascular damage often reduce blood flow, so red blood cells struggle to reach these regions. Plasma-dissolved oxygen, however, can still diffuse into ischemic tissue, allowing cells to receive oxygen even when circulation is compromised.
Clinically, this leads to three important effects:
- Oxygen reaches tissues despite poor blood flow
- Cellular oxygen availability improves
- Repair mechanisms activate at the tissue level
When tissue oxygen levels rise, well-documented biological responses follow. Stem cell activity increases, and angiogenesis begins, leading to the formation of new micro–blood vessels. Over time, this improves natural circulation and supports sustained healing. The underlying medical mechanism behind this pressure-driven process is explained step by step in How Does Hyperbaric Oxygen Therapy Work?
HBOT vs Oxygen Therapy – Clinical Use Comparison
When patients ask me which option is better, I explain that normal oxygen therapy and HBOT are not competing treatments. They serve different clinical purposes, and the difference lies in how oxygen is delivered inside the body. This distinction becomes clear when we look at pressure, oxygen depth, and healing impact.
HBOT vs Normal Oxygen Therapy – Clinical Comparison
| Aspect | Normal Oxygen Therapy | Hyperbaric Oxygen Therapy (HBOT) |
| Pressure | Normal atmospheric pressure | Increased pressure inside a chamber |
| Oxygen Depth | Limited mainly to blood | Delivered through blood and plasma |
| Tissue Reach | Restricted in damaged areas | Reaches deep and poorly supplied tissues |
| Healing Impact | Supportive | Therapeutic |
From a clinical standpoint, normal oxygen therapy is useful when the goal is to support blood oxygen levels during acute or short-term needs. Doctors consider HBOT when the goal shifts toward tissue-level healing, especially in areas with poor circulation or delayed recovery. The added pressure changes how far oxygen can travel and how effectively it supports biological repair.
This comparison often helps patients understand when routine oxygen support is sufficient and when therapeutic oxygen delivery becomes necessary.
When Doctors Prefer HBOT Over Normal Oxygen
In my clinical experience, the decision to use HBOT is not about whether hyperbaric oxygen is better than oxygen therapy in general. It is about recognising why HBOT works when oxygen therapy fails in certain medical situations. Doctors look for signs that oxygen is not reaching tissues effectively, even when standard oxygen support is already in place.
Normal oxygen therapy depends on circulation to deliver oxygen. When swelling, inflammation, or vascular damage blocks this pathway, increasing oxygen flow alone does not change outcomes. This is the point where pressure-based oxygen delivery becomes clinically relevant. For patients exploring supervised medical treatment and clinical application, detailed information is available on our Hyperbaric Oxygen Therapy in Delhi page.
Doctors typically consider HBOT when:
- Healing does not improve despite adequate oxygen support
- Tissue-level hypoxia persists
- Circulation limits oxygen delivery
This approach is most commonly applied in conditions such as:
- Non-healing wounds, where poor tissue oxygenation delays recovery
- Radiation injury, where blood vessels are damaged
- Chronic inflammation, where swelling restricts oxygen diffusion
The depth of oxygen delivery, not the amount given, makes the key difference. HBOT uses pressure to move oxygen beyond circulation limits and into affected tissues, which explains its role when routine oxygen therapy reaches its limit. The article HBOT Explained in Simple Medical Terms explains this clinical reasoning step by step.
Is HBOT a Replacement for Normal Oxygen Therapy?
No. HBOT is not a replacement for normal oxygen therapy. In medical practice, both are used for different purposes, and each has a clear role. Treating them as interchangeable would be clinically incorrect.
Normal oxygen therapy is primarily used for acute support. It helps stabilise oxygen levels in the blood during breathing difficulty, infections, or short-term oxygen deficiency. Its goal is immediate support, not long-term tissue repair.
Doctors use HBOT for regenerative healing when the problem lies in oxygen delivery rather than oxygen intake, especially in damaged or poorly supplied tissues. By using pressure, HBOT supports tissue repair, cellular recovery, and long-term healing processes.
In simple terms, doctors do not choose one over the other. They choose the right tool for the right goal. Oxygen therapy supports survival and stability, while HBOT supports recovery and regeneration. This distinction is essential for safe, effective, and evidence-based care.
Quick Summary – Oxygen Therapy vs HBOT
To bring everything together, here is the simplest way I summarise this comparison for patients and readers.
- Oxygen therapy provides surface-level support by improving oxygen levels in the blood.
- HBOT delivers pressure-driven oxygen that reaches tissues and supports cellular healing.
- The real difference lies in pressure and delivery depth, not in oxygen itself.
In short, oxygen therapy helps the body cope, while HBOT helps the body repair. This single distinction explains why their roles in medical care are very different.
Final Conclusion: Oxygen Therapy vs HBOT
The comparison between oxygen therapy vs HBOT shows that both treatments use oxygen, but their medical roles are very different. Oxygen therapy mainly supports the blood during acute or short-term needs, while HBOT uses pressure to deliver oxygen deeper, directly to tissues where healing processes take place.
This difference in pressure and delivery depth explains why HBOT is not a routine replacement for oxygen therapy, but a targeted option when tissue-level oxygenation becomes critical. Understanding how oxygen therapy vs HBOT actually works helps patients and clinicians choose the right approach, based on healing goals rather than assumptions.
FAQ – Oxygen Therapy vs HBOT
Oxygen therapy increases oxygen levels in the blood at normal pressure. HBOT uses increased pressure to push oxygen deeper into tissues and cells, where healing actually occurs.
No. Oxygen therapy provides supportive care at atmospheric pressure, while HBOT is a medical treatment that combines oxygen with pressure to improve tissue-level oxygen delivery.
Normal oxygen depends on blood flow to reach tissues. HBOT uses pressure to dissolve oxygen into plasma, allowing it to reach damaged or poorly supplied tissues even when circulation is limited.
Only to a limited extent. Without pressure, oxygen mostly stays bound to red blood cells and cannot reliably reach deeper or swollen tissues.
For non-healing or chronic wounds, yes. Oxygen cylinders support blood oxygen levels, while HBOT delivers oxygen directly to wound tissues, supporting repair and regeneration.
No. They serve different purposes. Oxygen therapy is used for acute support, while HBOT is used when tissue-level healing and regeneration are the goals.
No. The key difference is pressure. Pressure changes how oxygen behaves in the body and allows it to reach areas that normal oxygen therapy cannot.
HBOT primarily improves tissue oxygenation. Blood oxygen saturation may already be normal, but HBOT increases oxygen availability at the cellular level.
Yes. Many patients have normal blood oxygen levels but poor tissue oxygen delivery. HBOT addresses this gap by improving diffusion into tissues.
Doctors prefer oxygen therapy for short-term or acute situations such as breathing difficulty, infections, or temporary oxygen deficiency where tissue healing is not the primary concern.
Both are safe when used appropriately under medical supervision. The choice depends on the condition being treated, not on safety alone.
Pressure increases the diffusion gradient, allowing oxygen to dissolve into plasma and move from blood into tissues more effectively, even in areas with poor circulation.